Steps to compliance
CMS’ Final Rule for CY2022, includes a 2-year phased adjustment to the way clinicians document and bill for split/shared visits (shared E/M visits). This change impacts physician and Mid-Level Non-Physician Practitioners (NPP) reimbursement. The old, shared visits policy was first issued in 2004. The revised policy is intended to better conform with current clinical practices of medicine and the continued expansion of mid-level providers (NPP), Nurse Practitioners and Physician Assistants. Health systems and provider practices must understand the Conditions of Payment in this policy update and what providers must do to comply.
Conditions of Payment:
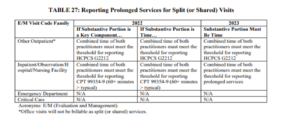
- Both phases of implementation will affect new and established patients, regardless of an initial or subsequent visit, including prolonged services. Note: this is for Professional claims and relevant only to those that are doing Provider Based Billing (PBB) through HB (Hospital Billing) in Epic. Prolonged services are defined in CPT codes 99354-99357: involving direct patient contact that goes beyond the usual (E/M) service (per CMS this does not apply to Emergency or Critical Care services). Table 27 from the CMS Newsroom press release.
- Each phase requires a modifier submitted on claims. Your PBO and Coding teams will want to ensure they have modified their workflows or added additional edits to ensure they are capturing the new FS modifier. FS Modifier was created solely for Split or Shared E/M visits; no additional definition for this modifier.
- The rule explicitly states, “Documentation in the medical record must identify the two individuals who performed the visit.” This also requires the provider doing the substantive portion of the services to sign and date the medical record.
Phase I
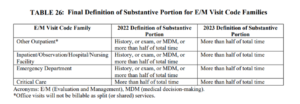
CY 2022, CMS updated the definition of split E/M Visits “as E/M visits provided in the facility setting by a physician and an NPP in the same group. The visit is billed by the physician or practitioner who provides the substantive portion of the visit.” The substantive portion is history, physical exam, medical decision-making, or more than half of the total time. (Table 26 from CMS below)
- This applies to Outpatient, Inpatient, Observation, Hospital, Nursing Facility, and Emergency Services.
- Critical care is only defined as more than half of the total time. (From Federal Register)
Prolonged services:
- Guidance if the Substantive is a key component or if the Substantive portion is time.
- Other Outpatient (office visits will not be billable as split (or shared) services):
- Combined time of both practitioners must meet the threshold for reporting HCPCS G2212
- Inpatient/ Observation/Hospital/Nursing Facilities
- Both practitioners must meet the threshold for reporting CPT 99354-9 (60+ minutes > typical)
Phase II
CY 2023, the rule provides further clarity on the substantive portion of the visit, “defined as more than half of the total time spent.”
- The guidance for Prolonged Services will move solely to Substantive Portion must be time still providing clear direction for Other Outpatient vs. Inpatient/ Observation/Hospital/Nursing Facilities.
Splitting and sharing the tasks around compliance with this new policy is a great approach; the following are suggestions from our Wilshire Revenue Integrity Team.
Convene a workgroup to manage this change. Include members from Revenue Integrity, Medical Director(s), Professional Billing team, Compliance, and Coding leadership as the governance group, and then pull in your clinical informatics and EMR application teams that support your professional services.
How to Do It
- RI (Revenue Integrity), Coding, and Corporate Compliance should review Split (or shared) visits policy and make revisions as needed. If you do not have one now would be the time to develop one.
- Coding and PBO to partner with IT (Information Technology) Systems team on developing the who/how the FS Modifier is added.
- Once you have completed the review of the policy, review and update current clinical documentation and charge workflows as needed. Pull in your clinical informatics, and provider teams to ensure the smooth modification and adoption of the changes.
- Leverage your coding educators and informatics teams to develop an education plan and the timeline for Providers / Mid-Levels and the coding team.
- RI (Revenue Integrity) and Professional Billing Leadership team should partner and develop an education plan for the billing/follow-up team to understand the required change to claims.
- Monitor Managed Care Payers for global policy changes including commercial services.
Once you complete your evaluation and implement the 2022 changes, it will be key to mark your teams’ calendars for September 2022 to prepare for Phase II of the Final Rule policy changes.
If your organization has any questions about this phased policy change, please do not hesitate to reach out to us at The Wilshire Group.